Definition
Coccygodynia, sometimes referred to as coccydynia, coccalgia, coccygeal neuralgia or tailbone pain, is the term used to describe the symptoms of pain that occur in the region of the coccyx.[1][2][3][4] The pain is most commonly triggered in a sitting position, but may also occur when the individual changes from a sitting to standing position.[3] Most cases will resolve within a few weeks to months, however for some patients the pain can become chronic, having negative impacts on quality of life.[3][4] For these individuals, management can be difficult due to the complex nature of coccygeal pain.[4]

Clinically Relevant Anatomy
The coccyx is a triangular bone that forms the most distal segment of the spine.[1][3] It is composed of 3 to 5 coccygeal segments.[2] These segments fuse together to form a single bone, with the exception of the first coccygeal segment.[2][3] The first coccygeal segment might not fuse together with the second coccygeal segment.[2][3]The ventral aspect of the coccyx is concave in shape, while the dorsal aspect of the coccyx is convex in shape.[1]The first coccygeal segment is composed of articular processes that form the coccygeal cornua.[1][2][4] The coccygeal cornua articulates with the sacral cornua of the inferior sacral apex of S5.[1][2][4] This articulation creates a symphysis or synovial joint, which forms one of the borders of the foramen for the dorsal branch of the fifth sacral nerve route (S5).[1][4]
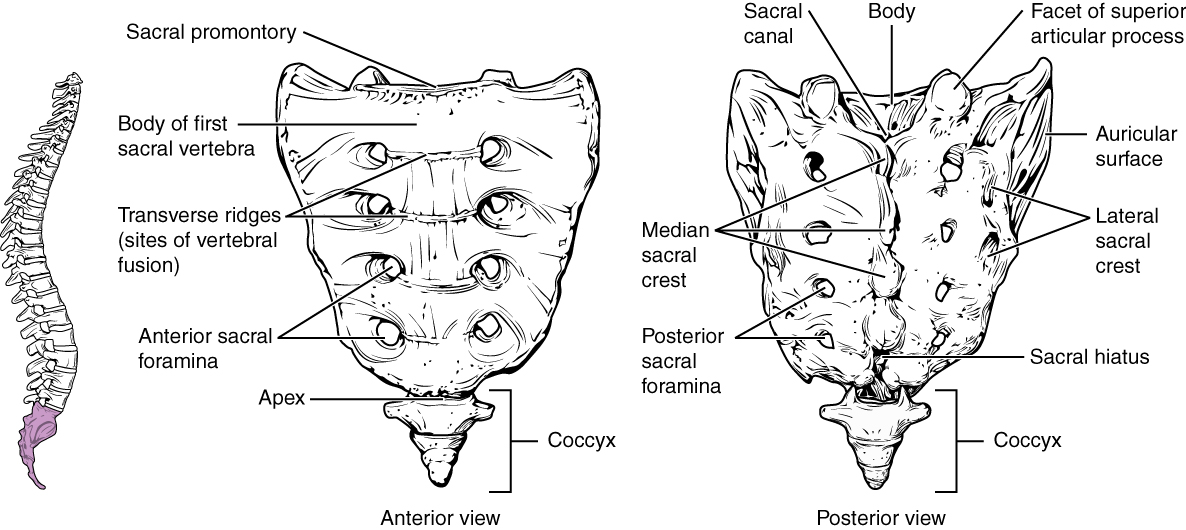
The coccyx serves as an attachment site for several muscles and ligaments.[4] Anteriorly, the coccyx is bordered by the levator ani muscle and the sacro-coccygeal ligament.[4] In an anterior (front) to posterior (back) direction, the lateral border of the coccyx serves as an insertion point for the coccygeal muscles, the sacrospinous ligament, the sacrotuberous ligament and the gluteus maximus.[4] Inferiorly, the tendon of the iliococcygeus muscle inserts onto the tip of the coccyx.[4]Together, these ligaments and muscles contribute to voluntary bowel control, as well, provide support to the pelvic floor.[4]
In addition to being an insertion site, the coccyx, in conjunction with the ischial tuberosities, provides weight-bearing support to an individual in a seated position.[4] For this reason, increased stress and pressure can be placed on the coccyx while a person leans back in a seated position.[4] The coccyx also functions in providing support to the anus.[4]
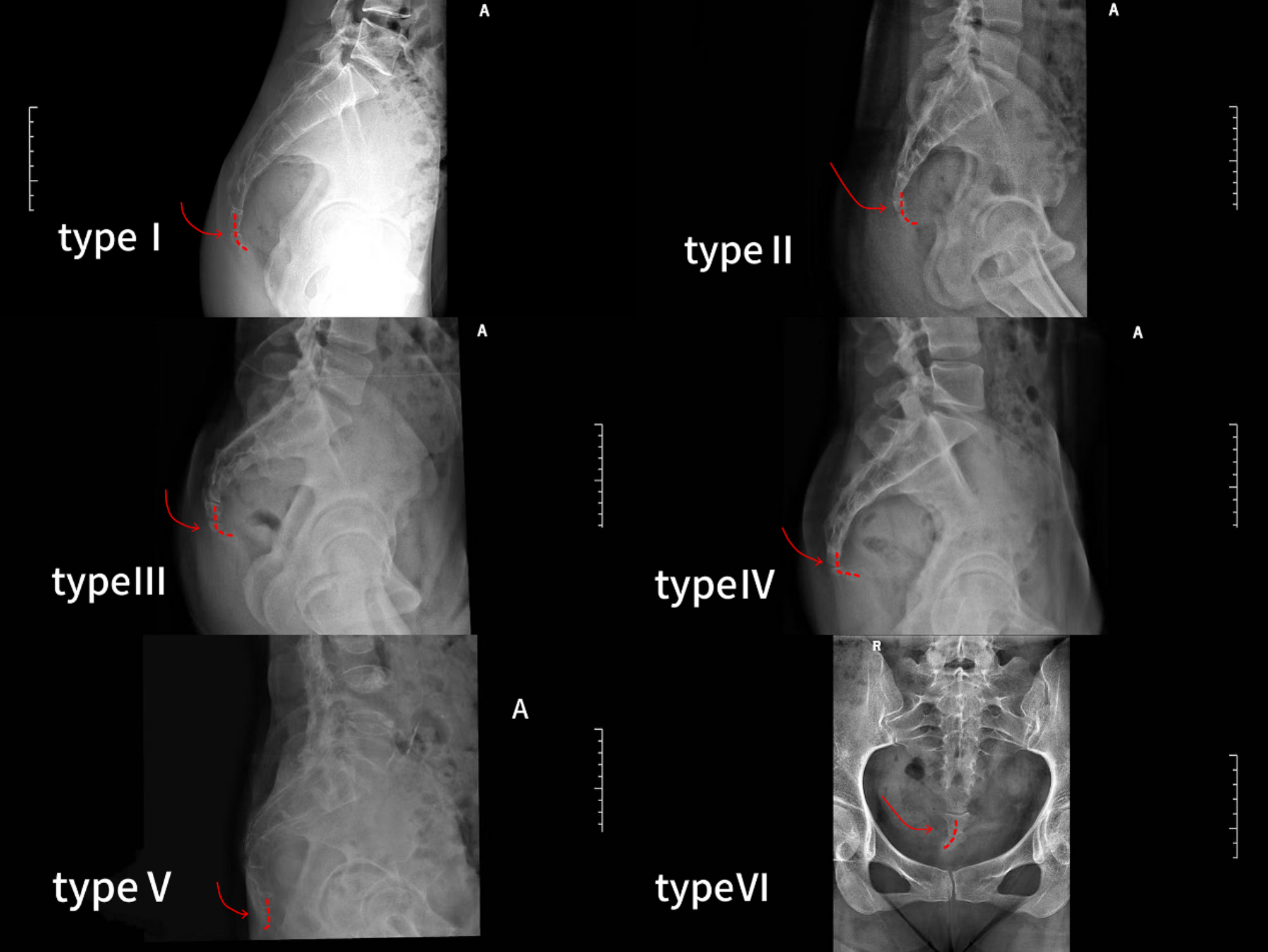
Postascchini and Massobrio (1983)[5] classified the variations in morphology of the coccyx into four different configurations:[5]
- Type I: The coccyx is slightly curved forward, with its apex positioned downward.[5]
- Type II: The forward curvature of the coccyx is more exaggerated, with the apex positioned in a straightforward direction.[5]
- Type III: Sharp angulation of the coccyx forward.[5]
- Type IV: Subluxation of the coccyx at the sacrococcygeal or intercoccygeal joint.[5]
Tailbone pain: How can I relieve it?
What causes tailbone pain, and how can I ease it?
Tailbone pain is pain in or around the bony structure at the bottom of the spine. This part of the spine is called the coccyx. Tailbone pain is sometimes called coccydynia or coccygodynia.
Tailbone pain can be caused by injury to the coccyx during a fall. It may also result from sitting for a long time on a hard or narrow surface. Other causes include joint changes from arthritis or during childbirth
- Lean forward while sitting down.
- Sit on a pressure-reduction cushion. Some people find a wedge-shaped one most helpful for reducing pain.
- Apply heat or ice to the affected area.
- Take pain relievers, such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others
Possible treatments for chronic tailbone pain might include:

- Surgery. Surgery can be done to remove the coccyx. The procedure is called a coccygectomy. This option is typically only recommended when all other treatments fail
- Physical therapy. A physical therapist might show you how to do pelvic floor relaxation techniques. One technique is breathing deeply and completely relaxing your pelvic floor — as you would while urinating or defecating.
- Manipulation. Massaging the muscles attached to the tailbone might help ease pain. Manipulation is typically done through the rectum.
- Medicine. An injection of a local anesthetic into the tailbone can relieve pain for a few weeks.
- Surgery. Surgery can be done to remove the coccyx. The procedure is called a coccygectomy. This option is typically only recommended when all other treatments fail
Epidemiology
No accurate data about the frequency of coccydynia is reported, but one study found that coccydynia accounted for ~3% of all low back pain hospital presentations 8. It is ~5x more common in females than males
Risk factors
- obesity 10
- female sex 10
- osteoporosis and other degenerative bone diseases ref
- osteomyelitis ref
- contact sports ref
- elderly with risk of fall
Radiographic features
MRI
- rigid coccyx with a spicule or spur at its tip
- bursa along the dorsal surface of the coccyx
- presence of fluid collection within the sacrococcygeal synchondrosis
- large draining vein on the ventral coccyx
- any inflammation or soft tissue abnormalities around the coccyx
Plain radiograph
Considered the first line of imaging of painful coccyx 10. Two types of radiographs:
- standard radiograph
- coccyx scoliotic deformity (AP and lateral)
- number and morphology of coccygeal segments including degenerative change
- useful radiological assessment to evaluate anterior angulation of the coccyx and its deformity
- coccyx scoliotic deformity (AP and lateral)
- dynamic sitting and standing radiographs 10
- superior to standard radiograph because it can detect measurement of the sagittal rotation of the pelvis and the coccygeal angle of incidence ref
- allows for assessment of coccygeal mobility by measuring the intercoccygeal angle with the generally accepted values being (although this is not validated/standardized) 10
- dynamic posterior intersegmental coccygeal subluxation 10
- <5°: immobile/rigid 10
- 5° to 25°: normal 10
- >25°: hypermobility 7,10
